Experiencing the menopause
Following our previous blog on managing the menopause, our Deputy Head of Education, Charlie Green (top left), speaks with friends to find out more about how they have been experiencing the menopause.
We hope this Q&A helps anyone going through the (peri)menopause.
With a total of 108 years of menstruation between our group of close friends, you would think we would have known what to expect from the menopause, but that wasn’t the case for each of us at first!
Despite all that experience, and all the trust and openness of long and supportive friendships, menopause – or should I say perimenopause – came as a surprise for many of us. Initially we withdrew, walked the road alone, often confused and anxious. It was unclear why we were suddenly finding life so tough and feeling disconnected from things we previously took pleasure in.
Perimenopause has often left each of us feeling disconnected from our lives and relationships.
But once one of us expanded their knowledge and started to share their experiences, we began to spot the symptoms in ourselves and in each other. We got better at reaching out and helping each other, which began to make everything easier.
So, we wanted to share some of our experiences, tips and stories with others who may be going through the menopause and may not have yet found people they can talk to or ask questions of. We hope you take some comfort, find some inspiration or feel more connected by reading our words.
Discovery: How did you find out you were perimenopausal?
“Before I reached out for help, it was all a bit dark. But after reading a news story about a lady who took her own life due to menopause symptoms, I took some action. I didn’t feel I could reach out to friends at that time, so I called a menopause specialist that morning.”
“I assumed a significant grief combined with the Covid-19 restrictions were the cause of my low mood, weight loss and anxiety. But 12 months after the grief I was still struggling so I called the doctor who gave me an unexpected prescription for hormone replacement therapy (HRT). I didn’t take it initially as I had unanswered questions. So, I started learning everything I could and sharing everything with friends.”
“As one of the youngest women in our group, I took my friend’s advice and was following the Dr Louise Newson podcast and tracking symptoms, so I spotted things early.”
“A friend noticed my dry eyes and we got talking about the menopause, and my learning journey began.”
“After discovering I was having to stay in bed for one or two days a month due to heavy and painful periods, a friend suggested I write down all my symptoms to share with the Women’s Health specialist who visits the doctor’s surgery once a month. I had about 15 symptoms on my list, all of which they acknowledged were likely connected to the menopause. I cried with relief at how good it was to feel understood and get help.”
“The fatigue, brain fog and poor memory have been so hard.”
Tough times: What was the hardest thing to deal with?
“Hot sweats at night and interrupted sleep, which leads to memory loss and brain fog.”
“Being undiagnosed for 18 months despite lots of visits to the doctor and severe symptoms.”
“The ‘Dragon’ who would sweep in with negative thoughts and feelings and who I did not recognise.”
“The fatigue, brain fog and poor memory have been so hard.”
“The tiredness and rage!”
“Struggling more with things like multitasking, which has always been a strong skill of mine. I now have to focus on one thing at a time, otherwise I don’t do anything very well. It’s been frustrating and an adjustment.”
“Feeling so hot! I just feel like my whole body temperature has increased. Hot summers can be really challenging.”
“Not finding joy where I previously did.”
“Pulling away from friends and family.”
“The social anxiety and not enjoying being around the people I love.”
“I just feel like my whole body temperature has increased.”
Unexpected: What symptoms did you have that you initially didn’t associate with menopause?
“Aching, sometimes painful muscles.”
“I wasn’t expecting to have such heavy periods.”
“Dry, sore eyes. I stopped wearing eye make-up and the eczema had come back around my eyes. It was like there was sandpaper in and around them.”
“Social anxiety in situations that should have felt comfortable.”
“Experiencing body odour which I never had before. Itching hands and feet, and forgetting words.”
“Painful joints that I assumed came with age. Now on HRT the pain has gone, and I am swimming one mile a few times a week and walking the dogs.”
“I forgot my HRT patch once and within 48 hours I fell out of love with myself, my job and my partner! Once the patch was back on, all was well in my world again quite quickly. That shocked me.”
“The insatiable rage over something as small as someone breathing near me or chewing!”
To HRT or not to HRT? That is the question
Please consult with your GP if you have any questions about medical treatments for menopause, as Suffolk Mind is not qualified to recommend one or another. Each person is different, so have included answers here to show the variety of experiences, rather than to provide advice.
“I am not taking HRT. I have started biking before work and at weekends. It has made a big difference in my weight and strength as well as my physical and mental health. The one symptom I really struggle with is the hot flushes at night. But I don’t know how my symptoms would be if I wasn’t as committed to the lifestyle choices.”
“I have the Minerva coil fitted for the progesterone and I take three pumps of Oestrgel per day in the evening. I have found this has really helped. My joints are not painful anymore, my eyes are soothed which is so lovely. I tend not to get brain fog so much, although do occasionally. I increased my dose from two to three pumps at the beginning of the year as I had some symptoms return.”
“I take Evorel (oestrogen) and Utrogestan (progesterone). It’s early days for me and I am on the lowest dose, but I feel they are benefitting me so far.”
“My symptoms are not too significant right now and I can manage them, so I run, eat well and make sure I do things I love. And I am always in bed by 9.30pm during the week. Sleep is key for me.”
“I have the pill injection (with progesterone), daily progesterone capsules with no break and four pumps of oestrogen gel daily. I increased over time from two to four pumps with advice from the women’s health nurse. I feel “me” again on my current dosage – all the symptoms have settled back down. The only thing left is that I feel a bit hotter than usual all of the time and can’t remember some words.”
“I have Utrogestan 100 (progesterone) and Oestrogen gel. Within 2 weeks I started to see the beauty again on my nature walks. I felt calmer and all symptoms dramatically reduced or left altogether.”
“I know HRT is not right for everyone and it is only one of the options, but for me it was incredibly positive. I can’t rely solely on replacing and balancing my hormones through HRT though. I have to keep focused on getting enough good quality sleep and eating well, as poor sleep, alcohol and a high sugar intake bring on some of the symptoms again.”
“I started to take HRT, but it didn’t work for me – I felt worse – so I stopped. I am now using food, sleep and movement to manage my symptoms and take lots of breaks. I have to avoid alcohol as it spikes my hot flushes.”
“I was really nervous to take HRT due to my family history, so I was really pleased to have a specialist nurse at our local surgery who could answer all my questions and give me links to research and information, so I could inform myself and make the right decision for me.”
“I had to try a number of different combinations of HRT before I found what worked and the symptoms got worse before they got better. I had been worried I was going to have to give up work as my brain was not functioning like it used to. But now, 16 months on, I am enjoying life again.”
“I use a combined HRT patch, which is working well now I am in a routine with them. Getting rid of the glue from the patches is literally a pain in the a***!”
Invaluable: Aside from prescriptions, what has been the greatest help for your health and wellbeing during this time?
“Morning routine of meditation and yoga, taking walks in nature and eating healthy nutritious food. But I must admit these practices did not ease me like they used to once I became perimenopausal. However, alongside HRT I feel they are now my saviour.”
“Reading and watching TV programmes on perimenopause, talking to others on their experiences. More work needs to be done on the impact of the menopause on those who experience it. There also needs to be more recognition of them in the workplace and the importance of their value, wisdom and experience and accommodating this life stage.”
“Talking to friends and reading the menopause doctor on social media and her book.”
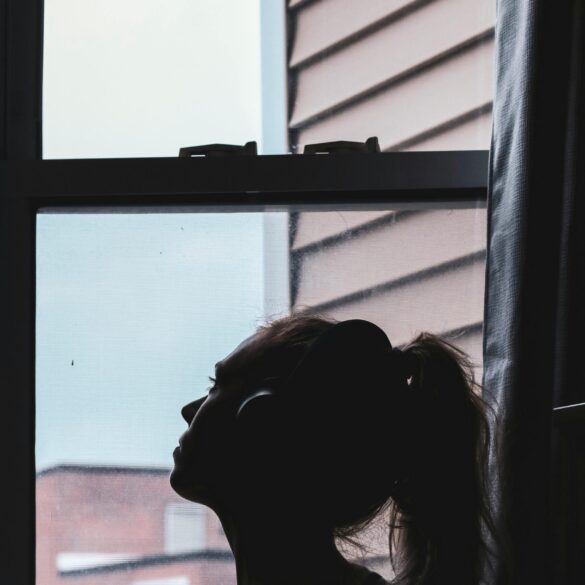
“Slowing down, finding opportunities to be in or near water and always having a fan in my bag! Having an understanding partner and line manager has also been such a relief – they have been so keen to learn more about it.”
“Being surrounded by women who are really open about their symptoms, challenges and treatment.”
“Having people I can talk to who have more experience and people who specialise in menopause.”
“Talking to friends, which helped me to realise it was something (in a weird way) to embrace. This then allowed me to deal with it rather than keep my head in the sand.”
“Movement each day, and time with my dog, is an important part of my self-care.”
“A walk on the beach or a dip in the sea can make everything feel better”.
Being by or in water can help to calm the mind and body
Unexpected upsides: What positives have come from your perimenopausal journey so far?
“Now I am the other side of the darkness, I sometimes feel I have increased inner strength and a deeper understanding of myself.”
“I have learned to value myself more. Pace myself. I look after myself better.”
“I am more aware of what I truly enjoy and value.”
“I feel I’ve been really lucky to have such a supportive and open group of female friends who are happy to talk about symptoms, share stories and support each other in tough times.”
“Having people around me who were able to spot symptoms that I had not associated with perimenopause.”
“Knowing myself better, saying yes to the things I want to do and confident ‘no’s to the things I don’t want to do.”
“Strangely enough, feeling the rage was quite liberating. Out of control, but liberating! Now I am on HRT I still try and spot things that would have caused the rage, because I wasn’t wrong to be cross about them, but now I try to do something more constructive about it!”
“Being unashamedly who you are. Being menopausal has encouraged myself and my peer group to be ourselves and not be as bothered by things like what other people think.”
“Meeting new people and sharing our stories proudly. This feels like a new and exciting time to be honest about what used to be a silent time of suffering for people experiencing the (peri)menopause firsthand. I hope all we are learning will help younger generations as they mature.”
Top tips: What advice would you give to other people experiencing symptoms?
- “Please reach out and ask for help if you feel you can. If, like me, your symptoms get dismissed by your GP, seek out another GP or guidance.”
- “Find a menopause specialist. Read Dr Newson’s work.”
- “Talk to a female GP early on in your journey.”
- “Track symptoms.”
- “Seek help and be pushy if you are not getting the help you think you need. Sadly, our wonderful NHS is still a little behind in terms of understanding symptoms and how to support, so be your own advocate! Push until you get what you need.”
- “Start by filling out this symptom checker from Suffolk Libraries, so when you go to see your healthcare specialist you can go armed with knowledge.”
- “If you’ve been ‘adulting’ as a human female for a while and you think you’ve finally got your head around what it means to be a woman, it’s probably time for you to go through the menopause. Hold tight and keep an open mind!”
- “Remember, if you are over the age of 45, you do not need a blood test and your periods do not need to have stopped to receive treatment. Treatment should be prescribed on symptoms. If you can cope with your symptoms, then keep doing what you are doing, but if they are preventing you from having a life that works, explore how treatment could help you.”
Thank you for taking the time to read our stories. We hope it has been helpful for you.
We encourage you to share this blog with your partner, children, colleagues and anyone else in your life who may benefit from knowing more about experiencing the menopause.
By sharing stories from real life, we can all help others on their journey through (peri)menopause and also help those around them to offer support with deeper understanding and compassion.
The menopause is a natural stage of life and the more we know, the easier we all travel through it.
What help is available from Suffolk Mind?
Suffolk Mind have partnered with Suffolk Libraries for the Menopause & Me project to support people experiencing the menopause, and the people around them.
Menopause & Me provides the following free services:
- Support for those with lived experience. A six-week course focuses on different areas of information and support, to help people better understand their symptoms, and how to support themselves
- Support for employers. A one-day session for small-medium business (less than 250 employees) focusing on raising awareness of the (peri)menopause, and how the effects and associated symptoms can be supported and managed within the workplace
- One-to-one employment support. If you are experiencing the menopause or perimenopause, Suffolk Mind can offer you a dedicated support worker through our Suffolk Work Well service